Aug. 21, 2021

Derek J. Lomas, M.D., Pharm.D., a urologist and specialist in focal therapy for prostate cancer at Mayo Clinic in Rochester, Minnesota, discusses the addition of high-intensity focused ultrasound (HIFU) to the prostate cancer focal treatment armamentarium.
Provide a little history: How did HIFU progress to a treatment for primary prostate cancer?
The first HIFU prostate cancer clinical trials, completed in the mid-1990s, showed that HIFU could ablate prostate tissue successfully. This finding led to additional studies, and HIFU ultimately entered clinical practice around the world during the following decade.
Initially, HIFU was used to perform whole-gland ablations for prostate cancer. While this application was successful, there was increasing interest in limiting prostate cancer treatment-related side effects by restricting the amount of the prostate that was treated. This treatment approach is termed focal therapy.
The goal of focal therapy is to treat only the area with the most aggressive tumor while leaving the rest of the prostate and its surrounding structures alone. This approach is widely accepted in other types of cancer. For example, we commonly treat kidney cancers by removing or ablating only the tumor while leaving the rest of the kidney intact.
The prostate tumor that is targeted is referred to as the index lesion. In prostates with more than one tumor, this is generally the largest tumor with the highest grade. In these cases, it is believed that the index lesion drives the behavior of the prostate cancer and that treating it alone with focal therapy may lead to good overall cancer control with fewer side effects.
What type of patient is particularly well suited for HIFU?
The ideal candidate for focal therapy typically has intermediate-risk prostate cancer located in only one area of the prostate. This location is determined by prostate magnetic resonance imaging (MRI) and targeted prostate biopsy. My ideal candidate for focal HIFU has a lesion in the posterior or lateral portion of the prostate, a small- to moderate-sized prostate, and no major prostate calcifications or large cysts.
What are the major contraindications to HIFU?
There are a few limitations to HIFU. The first is prostate volume or size. HIFU treatment is delivered through a probe in the rectum, and the treatment can only reach so far away from the rectum. If patients have large prostates and anterior tumors, the energy may not reach anterior enough to provide effective treatment and negative margins. Sometimes tumors in larger prostates can still be treated if the target tumor is in the posterior part of the prostate.
The next limitation is calcifications in the prostate, which are problematic for a couple of reasons. First, the ultrasound energy cannot travel through dense material such as calcifications, so any areas of the prostate behind these may be undertreated. Next, these calcifications can reflect the energy, which could potentially lead to unwanted heat being transferred back to the rectum.
Other potential contraindications include inflammatory bowel disease of the rectum, prior significant rectal surgery, inability to insert the transrectal probe into the rectum, urethral stricture or active infection.
How do you counsel patients who receive HIFU? What is the typical side effect and complication profile? What is the typical recovery?
Overall the focal HIFU procedure is very well tolerated. HIFU is done as an outpatient procedure with a same-day discharge. A Foley catheter is placed during the procedure and is usually left in place for 5 to 7 days following the procedure to allow post-treatment swelling of the prostate to subside.
Once the catheter is removed, most patients do have some temporary obstructive and irritative urinary signs and symptoms including urinary urgency, frequency, slower stream and dysuria. We can manage the signs and symptoms with medications, and patients typically get better within a few weeks.
Rates of new urinary incontinence and erectile dysfunction developing are generally lower than those with prostate removal surgery but are dependent on the location within the prostate being treated. Other side effects that can occur include urinary retention, urinary infection, ejaculatory dysfunction, urethral stricture and rectal fistula (rare).
Most men are able to resume general activities in 1 to 2 days, including regular short walks. More intense physical activity can be resumed once the catheter is removed. There are no incisions to care for or stitches to remove.
Briefly, what are the logistics of the delivery of HIFU?
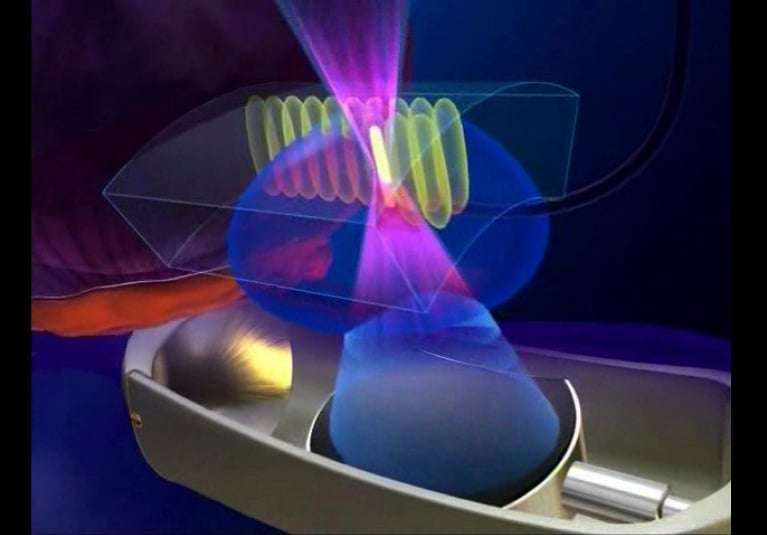
The HIFU procedure is done while the patient is under general anesthesia. Once the patient is completely anesthetized, a special ultrasound probe is placed in the rectum. There are no incisions or even any needles used. This ultrasound probe is used to both image the prostate and deliver the treatment. Once the initial positioning and planning steps are complete, treatment is delivered.
Each HIFU treatment lasts just a few seconds and destroys an area of tissue that is about the size of a grain of rice. An ablation zone is created by delivering multiple treatments to cover a predefined area of the prostate based on imaging and biopsy results. During the treatment, the surgeon is given real-time imaging as well as treatment parameters including temperature readings and calculated tissue changes to assess the quality and success of ablation. The procedure length depends on the size of the area to be ablated but in general takes approximately two hours.
How do you see HIFU playing a role in prostate cancer treatment over the next 10 years?
I see focal therapy in general becoming an option for more men in the next 10 years as more data supporting its use emerge and more providers become trained in the techniques. HIFU will definitely continue to be one of the main technologies used in prostate cancer focal therapy. There will continue to be ongoing research on other ablation technologies as well. To have a well-rounded focal therapy program, we must have multiple ablation technologies and techniques available to allow for focal therapy to be offered to a wide range of patients. There is still a role for radical prostatectomy and radiation therapy, and certainly they remain the standard of care at this point, but I think focal therapy should at least be part of the treatment discussion in men who are appropriate candidates and seeking a less invasive treatment option.
In recent years, a new treatment strategy known as focal therapy (partial gland ablation) has emerged for prostate cancer considered to be “intermediate risk” — mostly, small tumors confined to one area of the prostate. At Memorial Sloan Kettering Cancer Center (MSK), researchers have been working closely with an advanced focal therapy approach known as high-intensity focused ultrasound (HIFU), guided by magnetic resonance imaging (MRI).
Now a landmark clinical trial has demonstrated this less-invasive method works well for many patients. The phase 2 trial, led by MSK urologic cancer surgeon Behfar Ehdaie, looked at a particular type of HIFU treatment, also called MR-guided focused ultrasound (MRgFUS), in men with intermediate-risk cancer. The novel approach effectively controlled the disease in patients and greatly reduced adverse side effects of treatment. This suggests many men with intermediate-risk prostate cancer can avoid surgery, chemotherapy, and radiation.
“We believe this novel treatment strategy will improve the lives of many prostate cancer patients,” Dr. Ehdaie says. “Instead of removing all the tissue in the prostate, we have learned that it is safe and effective to treat specific areas and greatly reduce the burden on patients.”
Results from the clinical trial, published June 14, 2022, in Lancet Oncology, represent a major step toward having the new HIFU approach become part of widespread prostate cancer treatment.
When the cancer is confined to the prostate gland, the main treatment options have traditionally included active surveillance (close monitoring), surgery, and radiation. But men who needed surgery or radiation often had persistent side effects, such as urinary and sexual problems, that could reduce quality of life.
“Advancements in prostate cancer over the past two decades have been headlined by successes that have benefited all patients, and now focal therapy provides another exciting area that can move the needle in prostate cancer management,” Dr. Ehdaie says.
How Does HIFU for Prostate Cancer Work?
The MR-guided focused ultrasound (MRgFUS) is an outpatient treatment that takes about two hours. Patients under anesthesia are placed in an MRI machine that covers the lower half of the body. After the machine takes an image of the prostate, the doctors outline the treatment area and deliver the focused ultrasound waves, guided by the MRI. The ultrasound waves come from different directions, intersecting to attack and kill the cancer by heating the cells to more than 158 °F (70 °C).
We have demonstrated the procedure is safe for patients, and they can return to normal activity right away.
“While you are imaging, you are getting temperature feedback as well to make sure the right spots are being treated,” Dr. Ehdaie says. “The patient wakes up from the anesthesia and goes home. There’s no incisions or wounds on the body to heal. We have demonstrated the procedure is safe for patients, and they can return to normal activity right away.”
Prostate Cancer HIFU Treatment Patient Success Story
John Brannan is one of the success stories. In 2016, when he was 65, his prostate-specific antigen (PSA) began rising steeply. Although prostate cancer is largely not hereditary, he was alarmed because his father, uncle, and two cousins all died from the disease. A doctor in Boston suggested surgery to remove the cancer as soon as possible. But that night at a dinner party, John spoke with two of his wife’s friends who had surgery for prostate cancer and discussed some of the side effects that had persisted. One friend knew about the clinical trial and connected John with MSK medical oncologist Howard Scher, who referred him to Dr. Ehdaie.
John was eager to enroll. “In addition to personal reasons for wanting this treatment, I also hoped to help the next generation who might benefit,” he says. “I’ve seen the effect this disease can have on my own family.”

John Brannan, with wife Lita, called the HIFU treatment “a phenomenal use of technology.”
John says the process was easy. Dr. Ehdaie scheduled the MRgFUS treatment in the Center for Image-Guided Interventions at Memorial Hospital in September 2016. John walked out several hours later and went back to the hotel with his wife and had dinner. “It was pretty much back to normal right away,” he says. “No cutting, no stiches, no lying in a hospital bed for days or weeks. I wore a catheter for the first 24 hours and was a little tired, but that was it. The treatment was actually less painful than the biopsies I have had.”
Making HIFU Available for More Patients
Dr. Ehdaie says that using MRgFUS for intermediate-risk cancers became possible due to two important developments over the past 15 years. First, there was an acceptance by experts of using active surveillance for low-grade tumors. The second advance was new imaging technology that enabled MRIs to be incorporated into ultrasound treatment.
In the phase 2 clinical trial, 101 men received the novel MRgFUS treatment and then were biopsied six months and 24 months later. There was no intermediate- or higher-risk cancer left in the treated area for 88% of the patients.
“Probably most important was the lack of side effects,” Dr. Ehdaie says. “Nobody in the study reported urinary incontinence or experienced bowel problems. Most men were able to achieve erections.”
Based on this data, the FDA in December 2021 granted approval for the technology, called Exablate Prostate, to treat prostate tissue. The FDA also approved an investigator-initiated trial designed by Dr. Ehdaie and surgeon Peter Scardino to compare MRgFUS focal therapy to active surveillance and demonstrate a clinical benefit for patients with prostate cancer.
‘A New Lease on Life’
More than five years later, John is still doing well and has avoided surgery and radiation treatment. He has yearly follow-up checkups and periodic surveillance biopsies at MSK to make sure the disease has not returned. Now 70, he lives in Florida with his wife and stays active by buying and renovating properties.
Since his treatment, he has gotten calls from friends and acquaintances all over the country asking how they can get it too. MSK will be offering this novel treatment to select men and is hoping to launch the phase 3 clinical trial soon as well.
“I feel like I was given a new lease on life, so I’m trying to make the most of it,” John says. “It’s a phenomenal use of technology, and I think it’s going to absolutely take off across the world.”
Key Takeaways
- Men with intermediate-risk prostate cancer may not need surgery or radiation.
- A new approach uses high-intensity focused ultrasound (HIFU) to destroy prostate tumors.
- The treatment can control prostate cancer with greatly reduced side effects.
- This could change treatment for many prostate cancer patients.