Your physical therapist will perform a thorough examination that will include taking a full health history and observing you as you walk and perform the activity that causes your symptoms, such as running or jumping.
Your physical therapist will further perform a series of tests and measures of your musculoskeletal system that assess your strength, mobility, flexibility, and pain response. The most reliable symptom of MTSS is pain felt when pressure is applied to specific locations on the shin.
If the results of the examination suggest MTSS, your physical therapist will discuss with you the goals of treatment and develop a specialized rehabilitation program for you. If a more serious condition could be contributing to your pain, you may be referred to a physician for further tests.
Medial tibial stress syndrome (MTSS), commonly called “shin splints,” is a condition in which pain occurs over the shin bone (the tibia) with running or other sports-related activity. It is usually due to overuse and occurs in athletes who participate in repetitive activities, especially running and jumping. The condition can also develop in athletes who have suddenly increased the duration or intensity of their training. It is quite common and occurs more often in females.
What causes Medial Tibial Stress Syndrome?
Medial tibial stress syndrome develops when there is irritation where the calf muscles attach to the shin bone. It can also occur when running on a slanted surface or downhill, or when someone participates in a sport with frequent starts and stops. Training errors, shoe wear, and changes in training intensity, duration, and surface can contribute to the development of medial tibial stress syndrome. Risk factors for developing medial tibial stress syndrome include abnormalities of ankle and foot alignment, lower extremity flexibility, and strength.
What are the symptoms of Medial Tibial Stress Syndrome?
Most people complain of pain along the shin bone. The pain can range from a dull ache to a sharp, intense pain. Commonly, the pain is located along the inside border of the shin bone, usually in the middle or lower third. Pain may be present with early activity and subside with continued exercise, but may also persist throughout the activity. Typically, the pain goes away when the athlete rests, though in very severe cases, the pain can occur throughout the day (without activity) and continue even during rest. These more severe symptoms can also occur with stress fractures, a more serious injury.
How is Medial Tibial Stress Syndrome diagnosed?
Medial tibial stress syndrome is diagnosed based on a review of the patient’s history and physical examination of the lower leg. X-rays appear normal in people with shin splints. If the doctor is unsure of the diagnosis, an x-ray, MRI, or bone scan may be used to rule out a more serious condition, such as a stress fracture.
How is Medial Tibial Stress Syndrome treated?
Treatment includes a period of rest and modification of activities to allow the inflammation and pain to resolve. Ice can also be helpful, as well as anti-inflammatory medication. Physical therapy may be prescribed, with the patient following a lower extremity strengthening and stretching program. Some people benefit from special shoe inserts (orthotics) that redistribute pressures during activity.
References
Yates B, White S. The incidence and risk factors in the development of medial tibial stress syndrome among naval recruits. Am J Sports Med. 2004;32(3):772-80.
Reshef N, Guelich DR. Medial tibial stress syndrome. Clin Sports Med. 2012;31(2):273-90.
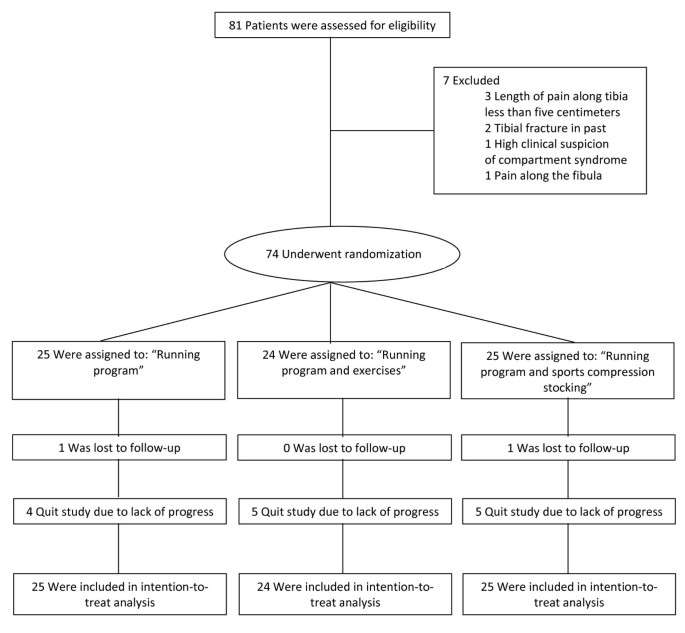
Subjects
The design of the study was a randomized multi-center trial with three groups. Each athlete was randomly assigned to a treatment group, and all the athletes in the group received an intervention. The multi-center study was announced to physical therapists, general practitioners, sports medicine physicians and orthopedic surgeons. They informed the athletes about the existence of the study. They could all refer an athlete to a sports physician in one of three participating sports medicine clinics in the Netherlands (two large district and one university hospital). The sports physicians examined the athlete for complaints of MTSS and for suitability for inclusion. If the athlete was suitable for inclusion, the sports physician referred the athlete to one of the investigators for intake. A single sports physician identically trained the investigators for the study. The diagnosis of MTSS was made according to the criteria of Yates et al. (see Table 1) [30]. For exclusion criteria the description of symptoms provided by Edwards et al. in their recent review were used to specify stress fractures of the tibia and chronic exertional compartment syndrome (CECS) [31]. Pain in stress fractures is often focal (clinically and with physical examination) and the start of complaints is usually abrupt. Pain initially occurs as a mild ache after exercise, but as the condition progresses pain can be felt early after starting exercise. Athletes with CECS often complain of burning, cramping or pain over the involved compartment with exercise. Pain is progressive with continued exercise and will disappear after cessation of activities [31].
Table 1 Inclusion and exclusion criteria
Full size table
The athletes had to be involved in sport at least once a week. The inclusion was definitive when the diagnosis MTSS by an instructed sports physician was confirmed according to the Yates et al. criteria [30] and the presence of exclusion criteria [31] was excluded (Table 1) and informed consent was given.
Randomization
For the randomization at each location there were three identical opaque blank envelopes in a box each containing a letter, explaining to which of the three groups the athlete had been allocated. After the athlete had been allocated the letter was returned to the envelope and into the box to be used again by the next athlete.
Intake
At baseline the investigators noted sex, weight, height, body mass index (BMI), kind of sport in which the athlete was involved, centimeters of pain on palpation of the postero-medial border of the tibia, side of the complaints and number of days with complaints. Subsequently, a running test was performed. The running test consisted of running on a treadmill at a fixed speed, while wearing the athlete’s own running shoes. Although the running test is not validated for the use in MTSS athletes it has been used previously in a treatment studies on MTSS [32, 33].
First, the athlete was shown a visual analogue scale (VAS) for pain by the investigators. Then the athlete was told that when a four (on a 1-10 VAS scale) for MTSS was experienced, defined as an indication that the pain was starting to become annoying, the running test had to be stopped. The running test started at 7,5 km/hour for two minutes. After this initial warming-up phase the distance was noted that could be run at 10 km/hour until a four on the VAS scale was noted. The distance ran at 7,5 km/hour was subtracted from the total meters run and was called “meters run at 10 km/h”.
Graded running program
With the result of the running test the athlete was placed in one of the six phases of the graded running program (see Table 2) [32, 33]. When “meters run at 10 km/hour” was between 0-400 meters, the athlete started the running program in phase one. When 401-800 meters could be run, the athlete started in phase two. When 801-1200 meters could be run the athlete started in phase three. When 1201-1600 meters could be run, the athlete started phase four. When 1600 meters or more could be run, athletes started phase five. When pain was present already during walking no running test was performed. Then the athlete was advised about how to avoid complaints by reducing loading of the leg. When in these athletes pain was not present during walking for two consecutive days, phase one of the running program was started. The running program was performed three times per week, with a day off between each session.
Table 2 Running program
Full size table
A new phase of the running program could be commenced if a phase was finished without a pain score of four or higher on the 1-10 VAS pain scale during the running. When pain (four or more on the VAS scale) was present immediately after the running or the day after the running the program did not progress and running remained in the same phase and the time run was decreased by two minutes.
Graded running program with exercises
In addition to the graded running, which is described above, athletes performed exercises at home five times per week (see addendum). The exercises consisted of stretching and strengthening exercises of the calves. The investigators practiced the exercises with the athletes until they were familiar enough to perform them at home. The exercise schedule consisted of five phases. When a certain phase could be performed without a four on a 0-10 VAS pain scale, the following phase could be started. When phase five was finished, the athlete kept on exercising with a random mix of exercises from different phases.
Graded running program with a sports compression stocking
In addition to the graded running program, which is described above, a sports compression stocking for the leg (Herzog Medical, Woudenberg, the Netherlands) was worn when the athlete was walking or running. The compression stocking could only be taken off when the athlete was seated or laying down for more than 15 minutes. To supply the right size, the investigators measured the circumference of the calf just below the knee fold, the maximal calf circumference and the circumference just above the malleoli. Based on these measurements a size 1-6 of the stockings was supplied.
Follow-up
Follow-up took place at week 2,4,6,8,10,12,16,22,28,34,42,50. To structure and perform follow-up, the investigators were identically trained by one sports physician (MM). Athletes were asked about progress with the running schedule, complaints and compliance with the treatment. Additionally, a physical examination was performed and feedback was provided.
Compliance
A commonly used method to measure compliance is self-reported adherence to the treatment [34, 35]. At follow-up athletes were asked to choose from the following sentences: “I stuck to the prescribed activities”, “most of the time I stuck to the prescribed activities”, “I stuck to the prescribed activities at the beginning, but not anymore”, or, “I did not follow the prescription at all” (adapted from Kallings et al., 2009) [34]. The athletes that answered “I stuck to the prescribed activities” and “most of the time I stuck to the prescribed activities”, when asked about the adherence of the prescribed activities, formed the group that adhered.
Blinding
The athletes and investigators were not blinded. The data analyst (EB) was blinded to the chosen therapy. The athlete was not blinded to the treatment, because it was not possible to perform blinding. The investigators were not blinded, because the investigators had to give feed-back to the athlete about the intervention. The investigators also asked about compliance of the prescribed treatment.
Outcome measurement
Primary outcome: the number of days from inclusion to the completion of phase six (being able to run 18 consecutive minutes outdoors at a speed in which speech becomes difficult) of the running schedule was used as primary outcome measurement. Although this outcome measurement was used in previous studies on the treatment of MTSS [32, 33], this outcome measurement has not been validated. Unfortunately, no validated outcome measurements for MTSS exist.
When an athlete was not able to finish the running program and quit the study, the Likert scale was used to assess the status of the athlete [36]. This scale was scored as: 1 = completely recovered, 2 = much improved, 3 = somewhat improved, 4 = same, 5 = worse and 6 = much worse. When a athlete did not have progress anymore and wanted to quit the study the Likert score was collected. The Likert scale was shown by the investigator and the investigator asked how the athlete was doing at the moment of quitting the study compared to baseline. The athlete chose a number. Satisfaction with the treatment in general on a 1-10 scale was used as secondary outcome measurement, in which 1 = very dissatisfied with treatment and 10 = highly satisfied with the treatment in general.
Data analysis
Data was entered using SPSS 17.0 (SPSS Inc, Chicago, Illinois, USA). To compare the outcome between groups Analysis of Variance (ANOVA) with post-hoc analysis according to Games-Howell was used. For dichotomized variables Chi-Square analysis was used. The athletes were analyzed by intention-to-treat. For athletes that were lost to follow-up a worst and best case scenario was calculated. For athletes that withdrew from the study due to a lack of progress, the time to complete the running program was entered as missing data in the database. Kaplan-Meier analysis was used to obtain reversed survival curves.
The local medical ethical committee agreed with the study beforehand (reference number for the study; NL23471.098.08). The committee agreed to include athletes who were 16 years of age and older. Informed consent was received from each participant.
Power analysis Previous studies on the treatment of MTSS reported a maximum time to recovery of 17.2 days and a standard deviation of 9,5 days [1, 9, 10]. Based on these findings, we considered a reduction of 50% in time to recovery would be clinically relevant. Sample size calculation indicated that 22 athletes (including an expected 10% lost to follow-up) per treatment group were needed to detect such difference with a power of 80% at a significance level of 0.05.