Medial Tibial Stress Syndrome or “shin splints” is a frustrating condition affecting millions of runners around the world each year. If you’ve ever felt achy, sore, or even burning discomfort along the inside of the shin bone, then you know it all too well. Today we’ll explain the research on this annoying running related injury and show you how to fix medial tibial stress syndrome (MTSS).
What causes MTSS?
Often, the pain of a running injury comes from one single tissue. If you have achilles tendonitis, for example, you feel the pain in the achilles tendon. Unfortunately, medial tibial stress syndrome is not that simple.
Although there is definitely variation between athletes, there are three different body systems that interact to cause the pain a runner feels in their shin. First, the tibia bone itself may have accumulated micro-trauma (minor structural damage to the bone) and be in the early stages of a stress reaction. A stress reaction is the first stage on a journey which can lead to a full stress fracture. Second, the periosteum (a membrane with lots of nerves that provides blood to the bones) around the tibia is also usually irritated, which can cause a runner to feel pain along the shin bone. And finally, the tendons of the lower leg, which run along the inside of the shin may also be overloaded and inflamed (summary of condition).
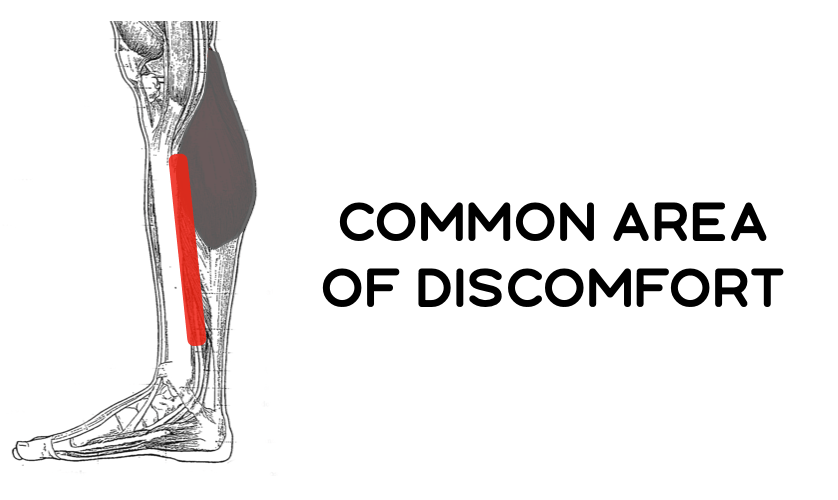
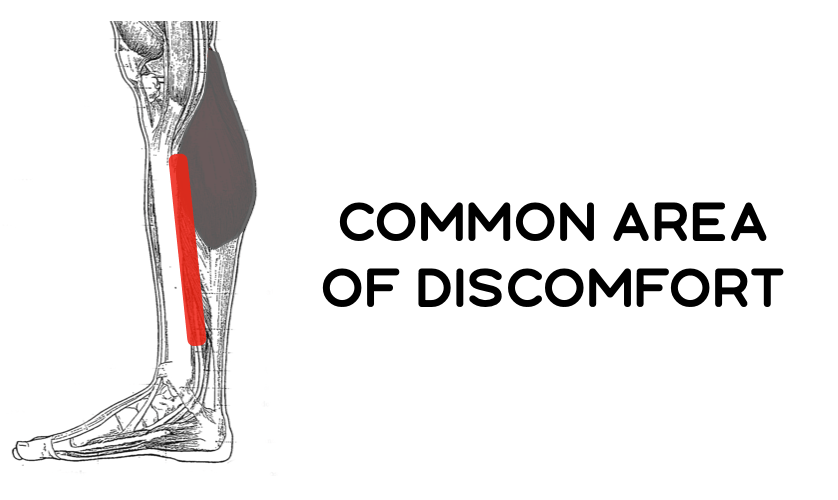
Long story short, some combination of the shin bone, the layer around the bone, and the tendons in the area are annoyed and sending pain signals to your brain. It is different with each athlete . This pain probably began to occur due to a combination of factors including training load, sleep, life stress outside of running, nutrition, and other things. Running injuries rarely happen for one simple reason.
How to fix medial tibial stress syndrome
Because Medial Tibial Stress Syndrome is different in each runner, most of the research done on MTSS has been of low quality and not produced treatments that drive consistent results (review). In fact, exercise therapy does not consistently beat other treatments, the way it does with almost every other running related injury. This makes sense, if an irritated tendon is the cause, strengthening exercises will be the best thing. If it’s a stress reaction, the a runner should rest. The trouble is in figuring out which is which or if something else may be going on.
Recover Athletics’ recommendations for runners with Medial Tibial Stress Syndrome:
- Temporarily reduce training load (total miles, pace, workouts), to see if things improve.
- Begin strengthening the muscles and tendons of the lower leg with the exercises shown below. There is never a downside in making your body stronger, and this may address the cause of your shin splints. Of course, this is different with each athlete.
- Ensure you’re getting enough calories & nutrients. In the offices of the world’s leading running researchers and physicians, any pain that involves a bone will often also involve speaking with a nutrition expert since bone health and nutrition are closely related.
- If things do not improve, please get checked out by a DPT or MD with expertise in running related injuries. If a bone stress injury is involved, they’ll be able to help you get back on track.
A simple exercise routine for medial tibial stress syndrome
Here are some exercises a runner could use to begin strengthening the muscles and tendons of the lower leg.
Exercise 1: Ankle Inversions with Resistance Bands


Why it works: This loads the muscles and tendons of the inner shin. This can be very beneficial if tendon problems are the source of your medial tibial stress syndrome.
Exercise 2: Calf Raises off Step


Why it works: the muscles of the calf intersect with tendons that may be involved in shin splint pain. Gradually making them stronger helps theses muscles process load better. Also, the health of this muscle is directly related to the health of the tibia. Improving one can help with the other.
Exercise 3: Standing Soleus Raises


Why it works: the tendons that attach to this muscle are almost certainly involved in any case of shin splints. Strengthening the soleus with this calf raise variation also helps improve the function of the entire lower leg.
You can try these exercises in the Recover Athletics app. The Recover App helps runners fix aches and pains and prevent injury. A year’s subscription costs less than one trip to physical therapist and we have an unlimited free trial. Give the app a try today!
If you don’t know us, we’re so glad you stopped by our page. Recover athletics is a team of runners, doctors, physical therapists, and entrepreneurs. We’ve made it our mission to help runners around the world prevent injury. Meet our team.
Our articles are not designed to replace medical advice. If you have an injury we recommend seeing a qualified health professional. To book an appointment with Tom Goom (AKA ‘The Running Physio’) visit our clinic page. We offer both in person assessments and online consultations.
It’s easy to talk generally with rehab, ‘strengthen x,y and z’, improve movement control etc but we don’t often expand on what exactly this means. Today’s blog is a brief look at an exercise programme I used recently for a patient with Medial Tibial Stress Syndrome and what my thinking was behind it.
The patient, in this case, is a young male middle-distance runner called Ben. He is, at this stage, pain free with all daily activities and running up to 40 minutes with no symptoms. He’s progressed nicely from the initial session where even jogging on the spot was painful, however, longer runs over 45 minutes cause some discomfort in the medial tibia. This has been a recurrent issue and Ben’s aim is to return to full training without these symptoms. He is gradually re-introducing high intensity sessions with guidance from his running coach and managing well. Assessment reveals mild weakness in Soleus, Glute Med and the posterior chain. Control of single leg balance and single leg dip is good and equal left and right. Ben works with an S&C Coach and is in the gym 3 days per week and is keen to have a number of exercises to work on.
Broadly speaking our aims are as follows:
- Improve local load capacity in the calf complex
- Improve kinetic chain load capacity considering the key muscles that aid in managing load
- Include weight-bearing exercises to improve bone load capacity
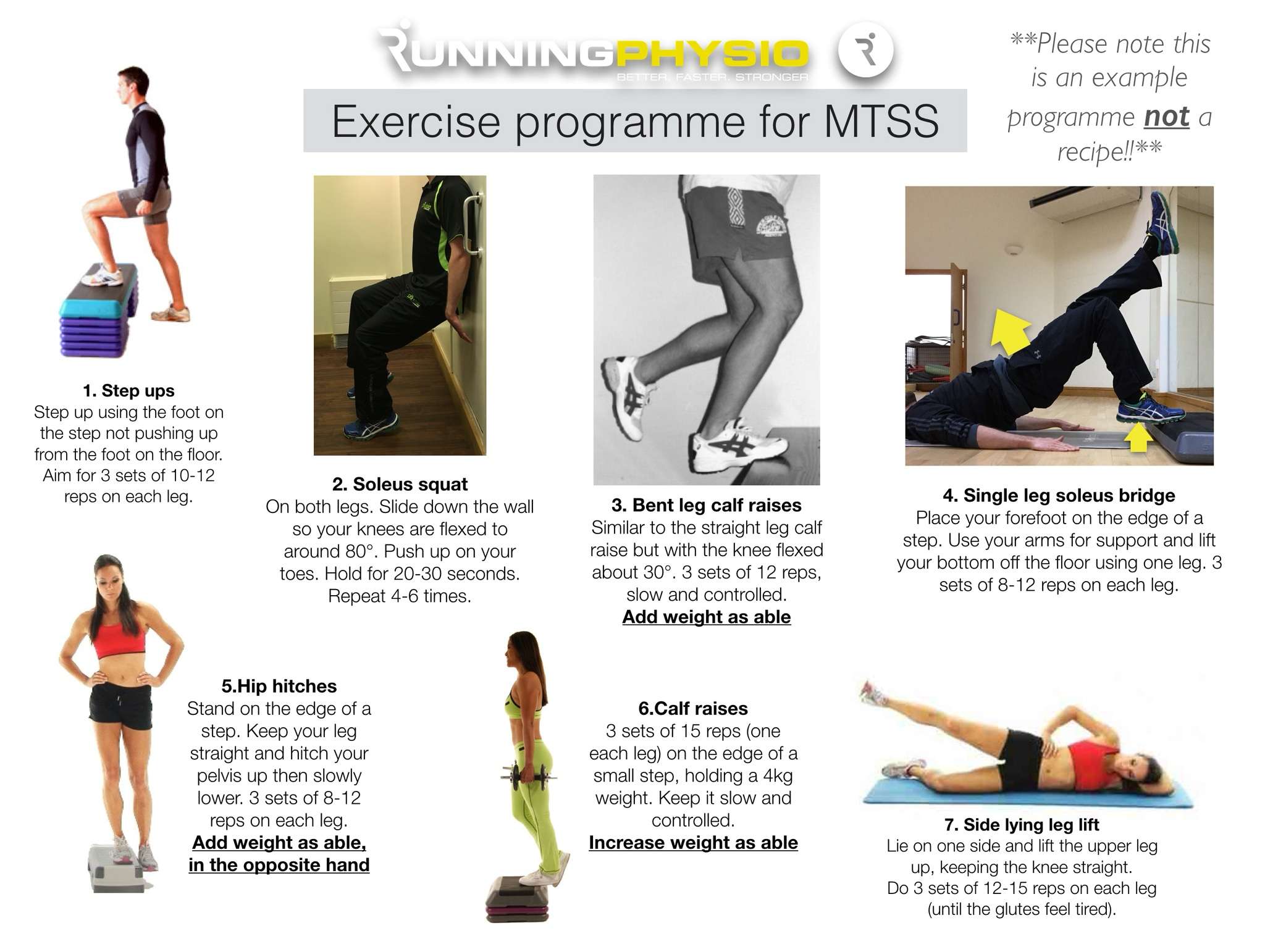
So Ben’s programme looks like this:
Let’s walk through each exercise.
1. Step ups
Simple but very effective! Step-ups achieve high levels of Glute Max activity (Reiman et al. 2012) as well as working Glute Med and providing a proprioceptive challenge. Gluteal muscles are vital in absorbing load during the stance phase of running. This exercise is first due to control aspect; doing this once fatigued from the other exercises may compromise movement quality. It is easy to progress or adapt to suit the patients changing needs.
2. Soleus squat
A nice isometric option that will challenge both the Soleus and Quads – 2 vital muscles in absorbing load during running. Hamner et al. (2010) found the quadriceps to be the greatest contributor to support.
3. Bent leg calf raise
A significant challenge to the calf complex especially Soleus. In MTSS Soleus is thought to be particularly important as it helps to reduce the bending force that the tibia experiences during impact which is thought to be key to the development of bone stress injury (Warden et al. 2014).
4. Single leg soleus bridge
Note this bridge is done with the forefoot on the edge of a step. The aim is 1) to lengthen the lever to challenge the posterior chain and 2) to work the soleus (again!). The soleus load may be fairly low but this will challenge Glute Max and the hamstrings. The hamstrings are most active during swing phase but they also contribute to the loading phase through co-contraction with the quads.
5. Hip hitches (AKA ‘Pelvic Drop’)
Ben’s assessment revealed Glute Med weakness and this is hoping to address this. EMG studies suggest high levels of Glute Med activity and we can use this emphasize a ‘high free hip’ to help reduce pelvic drop during loading. Adding load in the opposite hand is a simple progression.
6. Straight leg calf raises
These will strengthen gastroc and soleus. As indicated above a strong calf complex is important in reducing bone load in MTSS. Ben is a forefoot striker and research indicates higher loads for the calf complex in this group (Almonroeder et al. 2013). We want to ensure he has adequate strength to manage this load.
7. Side lying leg lift
This old chestnut works Glute Med with minimal anterior hip flexor activity (McBeth et al. 2012). It’s a fairly simple exercise for isolated Glute Med strengthening. We’ve worked the glutes in an exercise where hip and knee control is included (step up) and where pelvic movement is controlled (the hip hitch), now we’re isolating it and trying to work to fatigue to stimulate strength gains. I include this at the very end as once you’ve worked the glutes to fatigue it makes control of other exercises very challenging!
We’ve given Ben some indication of reps and sets but also suggested he works to fatigue within each set. The rep range is currently roughly 8 to 15 reps. We’re using fatigue here as a method to ensure he’s loading enough. If Ben isn’t reaching fatigue within this range he needs to make the exercise harder by adding load, increasing range or increasing time under tension. We’ve also suggested Ben works alternate legs – work to fatigue on the right then exercise the left leg while the right leg recovers.
Communication is important here – Ben is happy with his exercises and how to progress each of them. We’ve also discussed them with his S&C coach and kept his running coach up to speed on his progress and load tolerance so we can work together as an integrated team.
As I’ve mentioned in the exercise image above this is not a recipe for MTSS just a snapshot of one patient’s exercises and why we’ve used them. Ben’s rehab is reviewed, adapted and progressed at each session and is part of a comprehensive management programme including athlete education, gait re-training and a graded return to running.
I don’t think there’s a right way and a wrong way to prescribe exercises but it’s good to have a reasoning process and be open to feedback. I asked a good friend of mine, Sam Blanchard (@SJBPhysio_Sport) for his views on the programme. Sam is Head of Rehab Physiotherapy for Rochester Amerks, has an excellent blog and has published some great research on exercise selection and progression. He raised 3 key points;
- You don’t necessarily have to work to fatigue to get stronger and you’d want to consider the impact of working to fatigue on his running and other training sessions. When managing concurrent training evidence suggests not working to failure may be preferable for performance gains. It’s worth noting, however, the majority of this research is in healthy individuals, without injury.
- Muscle fatigue is thought to be a key factor in the development of bone stress injury. You may want to work proprioception or strengthen the glutes in a fatigued state which may simulate loading characteristics during longer runs.
- Impact work could be added as a progression to improve bone load capacity and active stiffness in the calf complex
Sam makes some great points and I agree, in particular, it is important to strike a balance between rehab and running. We’ve worked with Ben’s S&C and Running Coaches to develop a programme that allows adequate recovery between strength and running sessions. In addition, Ben has recently added low-level plyometric work to his rehab programme with an emphasis on controlled, comfortable impact. Sam was right on the money there!
Closing thoughts: exercise prescription for MTSS and other injuries requires an individualised approach considering how, when and where the athlete might do their rehab. It’s essential too that they know why they’re doing it and how it will help them achieve their goals. Not every patient will want an extensive programme; in fact, in many cases, 3 or 4 key exercises can be very effective. If you prescribe exercises try doing one of the programmes you’ve provided for a week – it’s much harder than you’d think! My final point is key…
…exercise prescription is all about reasoning, not recipes!
If you’d like to share an example of exercises you’ve used for a runner and your reasoning behind them please email your ideas to me, [email protected] and we’ll feature the best ones on the site!