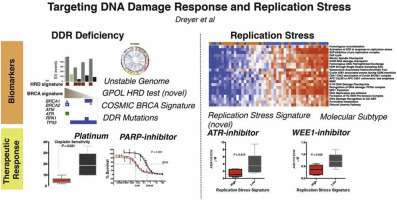
The identification of the underlying genetic alterations across all major subtypes of cancer has provided unprecedented insight into DNA repair proteins that are altered in cancer (26) and has laid the foundation for several precision medicine approaches. Almost every tumor has at least one gene in the replication stress response altered, providing ample opportunities to exploit tumor-specific alterations without affecting normal cells. The concept of synthetic lethality (73), whereby the presence of cancer-specific mutations in specific genes renders other genes essential for cell proliferation and survival, has been fundamental for the discovery of several of these gene-targeted strategies (74). Perhaps the best example of this strategy is the successful use of PARP inhibitors for the treatment of BRCA1/BRCA2-deficient breast and ovarian cancers, as these double-strand break repair defective tumors are dependent on PARP activity for cell survival (37, 75). Considerable effort is now being expended to identify additional synthetic lethal interactions with DNA repair genes, including replication stress response genes. One of the most promising targets currently being explored is ATR. Tumors harboring mutations in genes encoding the chromatin remodeler ARID1A or the DNA damage kinase ATM are synthetically sensitive to ATR inhibitors, with a complete response observed in a patient with metastatic ATM-deficient colorectal cancer (76–78). The dependency of ARID1A-deficient tumors on ATR has been attributed to the mitotic defects present in these cells, which causes an increased reliance on ATR function. Both ARID1A and ATM are frequently altered in tumors, particularly in ovarian and endometrial cancers for ARID1A and lymphoid malignancies for ATM, illustrating the applicability of these findings. In addition to further interactions with ATR, tumors containing mutations in other frequently altered replication stress response genes including RPA1 (NCT03207347 and NCT03377556) and the mutagenic DNA polymerase POLQ (79) are currently being explored to identify druggable synthetic lethal interactions. Genetic interactions with replication stress–inducing agents including CHK1 (80, 81) and WEE1 (82) inhibitors are also being investigated for use in mutation-specific tumor backgrounds, such as the use of CHK1 inhibitors in EZH2-deficient T-cell acute lymphoblastic leukemias.
Increased replication stress and cytosolic dsDNA in untreated KRAS mutant cancer cells
To investigate the role of mutant KRAS in DNA replication stress, we visualized replication tracts and measured fork speed and structures using the DNA fiber method (Fig. 1a). Cells were pulse-labeled with thymidine analogues CldU and IdU and lysed, and DNA fibers were spread and immunodetected with specific antibodies against CldU and IdU. First, we assessed the fork speed of fiber tracts in two isogenic KRASmut and KRAS wild-type (wt) cell pairs, NCI-H1703 and DLD1/DWT7 cells37. In both cell lines, the distribution of replication tract lengths was consistent with a slowing in fork progression in the presence of KRASmut (Fig. 1b,c, Suppl. Fig. S1A,B). Similarly, in a non-isogenic comparison for which four cancer cell lines were added, the average fork speed trended slower in KRASmut cell lines (Fig. 1d,e).
Figure 1
Baseline DNA replication stress and cytosolic DNA in KRAS mutant (mut) vs wild-type (wt) cancer cells. (a) Illustration of DNA fibers in exponentially growing cells that were pulse-labeled with thymidine analogues CldU and IdU and lysed after which DNA fibers were spread and immunodetected with specific antibodies against CldU and IdU. (b, c) Frequency distributions of DNA fiber length (i.e., CldU tract length) in isogenic cell pairs. (d, e) Velocity of fork progression in a panel of cancer cell lines (H1703, Calu-6 – lung cancer; DLD1/DWT7 – colon cancer; U2OS – osteosarcoma; MDA-MB231 – breast cancer; FaDu – head/neck cancer) and in a control (Ctrl) normal fibroblast line. (f, g) Percentage of fibers retaining only the first label (CldU) indicating fork stalling in isogenic cell pairs. (h) Percentage of bidirectional asymmetric forks that progressed through replication fork arrest. (i) Levels of double-stranded (ds) cytosolic DNA using PicoGreen dsDNA staining on cytosolic fractions from untreated cells. (j) Left, representative images of untreated cells stained with a dsDNA-specific antibody or DAPI. Right, semiquantification of fluorescent signal. All bars represent mean + /- SEM based on at least 3 independent repeats. Statistical comparisons by two-sided T-test indicating *p ≤ 0.05, **p ≤ 0.01, ***p ≤ 0.001.
Full size image
Next, we counted fibers that retained only the first label (CldU) indicating fork stalling. We found KRASmut cells having more fork stalling compared to wt cells though this was less pronounced in the DLD1/DWT7 cell pair (Fig. 1f,g). In addition to fork slowing and stalling, bidirectional asymmetric forks are also associated with replication stress. These derive from asymmetrical fork progression through replication fork arrest. KRASmut cells had significantly more bidirectional asymmetric forks compared to wt cells (Fig. 1h). Lastly, to measure the new origin firing rate during the second labeling (second pulse origins), we counted the number of new origins fired during the IdU pulse (green fiber signal only) and divided it by the overall origin firing rate (calculated as the total number of origin firing events during the first (green–red-green fiber signal) and second labeling pulse (Fig. 1a)). KRASmut cells exhibited variable second pulse origin firing depending on cell line (Suppl. Fig. S1C, D).
DNA replication stress and damage can cause accumulation of genomic DNA fragments in the cytoplasm of cells32,38. We focused here on assessing dsDNA content in the cytoplasmic fraction of live untreated KRASmut and wt NCI-H1703 cells using PicoGreen dsDNA dye (Suppl. Fig. S2A-C). This revealed a statistically significantly 15% higher signal in KRASmut compared to wt cells (Fig. 1i). To confirm this observation, we stained untreated KRASmut and wt cells for cytoplasmic dsDNA using a specific dsDNA antibody and subsequently analyzed single-cell fluorescent intensity (Suppl. Fig. S2D). Again, KRASmut cells had on average significantly more dsDNA (34% higher signal) (Fig. 1j). While this data is correlative it is consistent with the notion that replication stress in KRASmut cells is linked to cytosolic dsDNA production. Taken together, our observations provide insight into the replication stress phenotype of KRASmut cells, which confirms and extends previous findings on the cellular effects of oncogenic KRAS23,24.
Role of CHK1 kinase in regulating KRASmut-associated replication stress
RAS signaling has been linked to activation of the ATR-CHK1 pathway21,22,24,39. We, therefore, asked whether inhibition of CHK1 with LY2603618 (Suppl. Fig. S3A) would worsen replication stress and potentially yield a therapeutic opportunity in our isogenic model. CHK1 inhibitor was added during the second labeling. Assessment of fork speed showed that inhibition of CHK1 did not cause a substantial decrease of fork progression (Fig. 2a,b) and only a minor stalling of forks in KRASmut cells compared to wt cells (Fig. 2c). Anticipating that CHK1 inhibition would disrupt CHK1-mediated suppression of origin firing, we analyzed the effect of CHK1 inhibitor treatment on replication initiation measuring second pulse origins. The percentage of second pulse origins increased in both KRASmut and wt cells, with a larger increase in the presence of KRASmut, which is consistent with a more pronounced baseline CHK1 activity in these cells (Fig. 2d). As a result of replication stress, DSBs may occur due to fork collapse. Cells were treated with CHK1 inhibitor for 16 h, which produced higher levels of DSBs as measured by γ-H2AX foci in KRASmut cells compared to wt cells (Fig. 2e). However, CHK1 inhibitor monotherapy did not cause selective cytotoxicity (Suppl. Fig. S3B), indicating that alternative therapeutic approaches are needed to target the replication stress phenotype of KRASmut cancer cells.
Figure 2
Impact of CHK1 kinase inhibition on replication stress in KRAS mutant (mut) vs wild-type (wt) cancer cells. (a) Representative immunofluorescence images depicting the effects of pharmacological CHK1 inhibition (Chk1i) with LY2603618 (1 µM) during the second label (IdU) in isogenic NCI-H1703 cancer cells. (b) Frequency distributions of DNA fiber length with and without LY2603618 treatment. (c) Percentage of fibers indicating stalled forks. (d) Percentage of the ratio of new origins fired during the second label (ldU) and overall origin firings during both pulses. (e) Left, representative immunofluorescence images showing nuclear γ-H2AX and DAPI staining in Chk1 inhibitor-treated cells. Right, percentage of cells with at least 5 γ-H2AX foci following 16 h of treatment with LY2603618. All bars represent mean + /- SEM based on 3 independent repeats. Statistical comparisons by two-sided T-test indicating *p ≤ 0.05, **p ≤ 0.01, ***p ≤ 0.001.
Full size image
Resistance of KRASmut cells to exogenous replication stressors
To determine whether endogenous replication stress in KRASmut cells could be therapeutically targeted, we treated cells with hydroxyurea (HU), which depletes cells of dNTPs initially resulting in stalled replication forks. Cells were treated with 2 mM HU for 2 h in between pulse labeling (Fig. 3a). In KRASmut cells, no further increase in replication stress above baseline was observed while in KRASwt cells HU led to significantly slower fork progression and increased fork stalling (Fig. 3a–c). To exclude the possibility that this finding was due to a KRAS effect on dNTP metabolism, we also treated cells with the topoisomerase I poison camptothecin (CPT). Similar to HU, CPT treatment led to greater exogenous replication stress in KRASwt cells than in KRASmut cells (Fig. 3d, Suppl. Fig. S3C-F). In addition, comparable observations were made in DLD1/DWT7 cells (Fig. 3e,f, Suppl. Fig. S3G).
Figure 3
Resistance of KRAS mutant (mut) but not wild-type (wt) cancer cells to hydroxyurea (HU). (a) Distribution of fiber length in the isogenic NCI-H1703 pair with and without HU treatment (2 mM) administered for 2 h in between pulse labels. (b) Velocity of fork progression with and without HU treatment. (c, d) Percentage of fibers indicating fork stalling with/without 2 h treatment with HU or the topoisomerase I inhibitor camptothecin (CPT). (e, f) Distribution of fiber length and percentage of fork stalling in isogenic DLD1/DWT7 cells, analogous to panels A and B. (g, h) Combined effects of treatment with HU and CHK1 inhibitor (Chk1i) LY2603618 on fork stalling or γ-H2AX foci formation. All bars represent mean + /- SEM based on at least 3 independent repeats. Statistical comparisons by two-sided T-test indicating *p ≤ 0.05, **p ≤ 0.01, ***p ≤ 0.001; ns, not significant.
Full size image
Interestingly, CHK1 inhibition overcame the resistance of replication stress to HU in KRASmut cells (Fig. 3g, Suppl. Fig. S3G), which trended toward a correlation with higher levels of γ-H2AX foci after longer HU exposure (24 h) (Fig. 3h). However, when combining exogenous replication stress with CHK1 inhibition only mildly increased cytotoxicity was seen for KRASmut cells (Suppl. Fig. S3H). Taken together, despite their increased baseline replication stress KRASmut cells are largely resistant to exogenous replication stressors such as HU or CPT, which appears to be dependent at least in part on CHK1.
Cytosolic dsDNA induction as a function of KRAS status
Next, we asked whether the observed resistance of KRASmut cells to exogenous replication stressors would also result in a blunted cytosolic dsDNA production. We initially utilized radiation treatment with X-rays, which not only is linked to replication stress but also acts a potent inducer of cytosolic DNA27,33. To confirm our ability to detect radiation-induced cytosolic DNA, we first reproduced the radiation dose response that was seen in MDA-MB-231 cells in a recent study by Sylvia Formenti and colleagues, as shown in Fig. 4a33. Similarly, we found that 10 Gy irradiation caused on average a 1.4-fold higher dsDNA signal compared to baseline. A comparable 5 and 10 Gy dose response was seen in NCI-H1703 cells (Fig. 4b), yet the induction of dsDNA was less pronounced in the KRASmut clone compared to wt cells, i.e., statistically significant 1.07-fold lower induction after 10 Gy (Fig. 4b). At the same time, replication fork progression in KRASmut cells was not slowed by radiation in contrast to KRASwt cells (Suppl. Fig. S4A). A similar observation was made in KRASmut DLD1 cells in which cytosolic dsDNA induction was 1.12-fold lower than in wt cells following 10 Gy irradiation, though this difference did not reach statistical significance (Fig. 4c). A second assay in NCI-H1703 cells also found a numerically lower dsDNA induction of 1.08-fold (Fig. 4d).
Figure 4
Response of cytosolic dsDNA to exogenous stressors in KRAS mutant (mut) and wild-type (wt) cancer cells. (a) Levels of dsDNA using PicoGreen dsDNA staining on cytosolic fractions from KRASmut MDA-MB-231 cancer cells 24 h after treatment with increasing single doses of ionizing radiation (IR), i.e., X-rays. (b, c) Normalized levels of cytosolic dsDNA in isogenic cell pairs. Fold-difference in dsDNA induction at the highest dose is shown. (d) Left, representative images of untreated cells stained with a dsDNA-specific antibody or DAPI. Right, semi-quantification of fluorescent signal. (e) Screen of isogenic NCI-H1703 cells with replication stress inducing anti-cancer treatments HU (2 mM), pemetrexed (0.2 µM), cisplatin (20 µM), olaparib (5 µM), and proton radiation (10 Gy) showing normalized levels of dsDNA based on 1–6 repeats. Bars represent mean + /- SEM based on 3 independent repeats except where indicated. Statistical comparisons by two-sided T-test indicating *p ≤ 0.05, **p ≤ 0.01, ***p ≤ 0.001 (absence of these indicators signifies p > 0.05).
Full size image
We next screened additional replication-targeted agents to further confirm the reduced ability of KRASmut cells to induce cytosolic dsDNA in response to genotoxic treatments, which appeared to correlate with the observed exogenous replication stress resistance (Fig. 3). Treatment with different anti-cancer agents, including HU, again revealed numerically lower dsDNA induction in KRASmut cells compared to wt cells (range, 1.02–1.44-fold) (Fig. 4e). Interestingly, proton radiation appeared to be an exception to this (Fig. 4e) although we note that the differences in this screen were not associated with statistical significance.
Proton radiation targets the replication stress phenotype of KRASmut cells
Data from us and others have suggested that proton-induced complex DNA damages are particularly toxic to cancer cells with defects in homologous recombination and associated repair pathways35,36,40,41,42. However, the effects of proton irradiation on cells exhibiting replication stress are unknown. Given the unexpected finding in Fig. 4e with regard to the ability of proton radiation to induce cytosolic dsDNA in KRASmut cells, we returned to study the replication response of KRASmut and wt cells to proton treatment. Cells were treated with 2 Gy X-rays or protons between CldU and IdU labeling (Fig. 5a). Proton treatment conditions did not affect the replication stress phenotype of KRAS mut cells (Suppl. Figure 4B,C). We also previously confirmed that cell growth was not affected by the experimental set up35. The distribution of fiber tract lengths in KRASmut NCI-H1703 cells revealed a markedly more pronounced shortening in length after proton than after X-irradiation (Fig. 5a). In contrast, in KRASwt cells the distribution curves almost completely overlapped. A comparable differential effect of proton vs X-ray treatment was seen in KRASmut Calu-6 cells (Fig. 5a, Suppl. Fig. S4D). Consistent with these findings there was reduced fork speed, increased fork stalling, and asymmetric fork progression after proton irradiation in both KRASmut NCI-H1703 and Calu-6 cell lines (Fig. 5b–d, Suppl. Fig. S4E, F). Furthermore, there also appeared to be a differential dependence on CHK1 after treatment with X-rays versus protons (Suppl. Fig. S5A-C) though the exact functions of CHK1 in the response to damage from these two radiation modalities remain to be elucidated.
Figure 5
Cellular response of KRAS mutant (mut) and wild-type (wt) cancer cells to treatment with radiation or PARP inhibition (PARPi). (a) Left, representative images illustrating single DNA fibers following irradiation with 2 Gy X-rays (X) or protons (P) delivered in between pulse labels. Right, distribution of fiber length in irradiated KRASmut and wt cells. (b–d) Velocity of fork progression, percentage of stalled forks, and percentage of bidirectional asymmetric first pulse origins in isogenic cells irradiated with 2 Gy. (e) Fraction of cells surviving 5 days following irradiation with 6 Gy using a validated 3D viability assay14. (f–h) Velocity of fork progression, percentage of stalled forks, and percentage of bidirectional asymmetric first pulse origins in isogenic cells treated with/without PARPi olaparib (5 µM). (i) Fraction of cells surviving after 5 days of treatment with varying concentrations of olaparib. The drug concentration to achieve 50% cell survival (IC50) is indicated. All bars represent mean + /- SEM based on 2–3 independent repeats. Statistical comparisons by two-sided T-test indicating *p ≤ 0.05, **p ≤ 0.01, ***p ≤ 0.001; ns, not significant.
Full size image
Next, we asked whether increased replication stress following proton irradiation might correlate with enhanced radiosensitivity. KRASmut status is associated with radioresistance in vitro and in vivo as previously described by us and others13,14,15,16,43,44. Accordingly, both X-ray and proton irradiation was more toxic in the presence of KRASwt (Fig. 5e). Interestingly, the radioresistance of KRASmut cells appeared somewhat less pronounced after protons than after X-rays, i.e., 1.66-fold vs 1.87-fold more resistant than wt cells. However, the data also suggests that replication stress associated with proton irradiation was not sufficient to fully overcome the radioresistance of KRASmut cells. Taken together, our data indicates a different biology following proton vs. X-ray treatment that is revealed in the setting of pre-existing replication stress in KRASmut cells.
Proton irradiation and PARP1 inhibition have preferential cytotoxic effects in cells with defects in certain DNA repair pathways such as homologous recombination35,36. However, as DNA damages caused by these two treatments are different we sought to compare the replication response to protons with that to the PARP inhibitor olaparib. Interestingly, in KRASmut cells olaparib increased fork speed and did not induce fork stalling or bidirectional asymmetric fork progression, as reported in other cell models45, while the opposite was seen in KRASwt cells (Fig. 5f–h). Olaparib was mildly more toxic to KRASmut cells compared to wt cells (Fig. 5i) but overall these cells remained essentially resistant to PARP inhibition when compared to homologous recombination-defective cell lines (not shown). Lastly, recent data suggested that combined CHK1 and PARP inhibitor treatment is preferentially toxic to KRASmut HTC116 cells23; however, we did not observe any differential cell kill when these inhibitors were combined, possibly highlighting inter-tumoral differences across KRASmut cancers (Suppl. Fig. S5D).