The ability to adapt to environmental stress, including therapeutic insult, contributes to tumor evolution and drug resistance. In suboptimal conditions, the integrated stress response (ISR) promotes survival by dampening cytosolic translation. We show that ISR-dependent survival also relies on a concomitant up-regulation of mitochondrial protein synthesis, a vulnerability that can be exploited using mitoribosome-targeting antibiotics. Accordingly, such agents sensitized to MAPK inhibition, thus preventing the development of resistance in BRAF V600E melanoma models. Additionally, this treatment compromised the growth of melanomas that exhibited elevated ISR activity and resistance to both immunotherapy and targeted therapy. In keeping with this, pharmacological inactivation of ISR, or silencing of ATF4, rescued the antitumoral response to the tetracyclines. Moreover, a melanoma patient exposed to doxycycline experienced complete and long-lasting response of a treatment-resistant lesion. Our study indicates that the repurposing of mitoribosome-targeting antibiotics offers a rational salvage strategy for targeted therapy in BRAF mutant melanoma and a therapeutic option for NRAS-driven and immunotherapy-resistant tumors.
Together, these findings indicate that targeting mitochondrial translation with antibiotics of the tetracycline family should be exploited to rationally design anticancer therapeutic regimens. Importantly, given the widespread clinical use of such agents, these approaches could be rapidly implemented into the clinic.
Although the metabolic profile of cancer cells varies across patients, tumor types, and subclones within a tumor, there is emerging evidence that mitochondrial bioenergetics, biosynthesis, and signaling are required for tumorigenesis. Accordingly, several recent studies have demonstrated that mitochondrial biology is potentially a promising new area for cancer therapy ( Weinberg and Chandel, 2015 ; Jagust et al., 2019 ). Critically, as our understanding of the biology of MRD across multiple tumor types increases, it is becoming clear that DTP cells exhibit a strong dependence on mitochondrial biology, even higher than that of their drug-naive counterparts ( Jagust et al., 2019 ; Sharon et al., 2019 ; Davis et al., 2020 ). For instance, relapse-initiating cells in B-progenitor acute lymphoblastic leukemia are characterized by elevated levels of mitochondrial metabolism ( Dobson et al., 2020 ). Similarly, a slow-cycling population of melanoma cells that emerge in cultures exposed to vemurafenib or cisplatin exhibits elevated oxidative phosphorylation, and targeting mitochondrial respiration blocks their emergence and delays drug resistance ( Roesch et al., 2013 ). It remains unclear, however, whether metabolic reprogramming is the only underlying cause of this increased mitochondrial dependence and whether (all) DTP cells that coemerge following BRAF and MAPK kinase (MEK) coinhibition are equally sensitive to mitochondria-targeting agents.
Overcoming resistance to cancer therapy remains a major clinical challenge. Despite recent breakthroughs in targeted therapy and immune checkpoint blockade (ICB; Sosman et al., 2012 ; Larkin et al., 2015 ), the clinical response to these therapies is often incomplete and/or transient. These findings indicate that combining various therapeutic agents and modalities will be needed to overcome treatment resistance ( Holohan et al., 2013 ). Given that the development of new drugs is very slow ( Pushpakom et al., 2019 ) and is affected by high attrition rates ( Waring et al., 2015 ), the repurposing of existing de-risked compounds offers a fast track for the clinical implementation of novel and high-order drug combinations. However, a deeper understanding of the mechanisms underlying drug resistance is essential before novel combinations can be rationally designed.
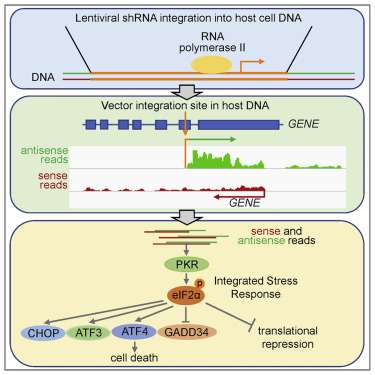
Overall, these data identify mitochondrial translation as a putative Achilles’ heel of cells engaging the ISR pathway, such as drug-tolerant cells. Of note, ISR signaling is activated not only in response to drug treatment: western blot analysis detected activation of the ISR, as demonstrated by the detection of P-eIF2α, ATF4, and C/EBP homologous protein (CHOP), in non–drug-exposed human melanoma lesions, including lesions that were resistant to both targeted and immune therapies ( Fig. 1 G ). These data therefore indicate that targeting mitochondrial translation may offer a promising therapeutic approach in a substantial number of patients/cases.
Strikingly, in silico analysis highlighted that 69.3% (122 of 176) of all ribosome-bound mRNAs in salubrinal-treated cells contain G-quadruplexes (rG4s; P = 2.4 × 10 05 Benjamini–Hochberg corrected value; Fig. 1, E and F ). In keeping with this, validated and/or predicted rG4s were identified in 88% (15 of 17) of the ribosome-associated mRNAs encoding mitochondrial proteins. rG4s, which are noncanonical four-stranded structures formed by guanine-rich sequences, have been implicated in all steps of RNA metabolism ( Dumas et al., 2021 ). The above observations suggest that rG4s may contribute to the specific recruitment of selected transcripts to the translation machinery in cells undergoing ISR ( Fig. 1, E and F ).
Considering that mitochondrial translation adapts to the influx of nuclear-encoded mitochondrial proteins, the observation that drug-tolerant cells down-regulate cytosolic protein synthesis suggests that these cells may also reduce the activity of their mitochondrial translation machinery. Surprisingly, however, puromycin incorporation assay followed by mitoplast isolation upon salubrinal treatment demonstrated that ISR activation caused instead a dramatic increase in mitochondrial translation, despite the expected overall decrease in cytosolic translation ( Fig. 1, B and C ). To further investigate the underlying mechanism, we identified translationally regulated mRNAs upon salubrinal treatment by performing polysome profiling analyses followed by RNA sequencing. We identified 382 transcripts whose association with ribosomes significantly (adjusted P value <0.05) changed in response to ISR activation and thus in response to phenotype switching and acquisition of therapy resistance. As expected, the vast majority of the transcripts (90%) were depleted from the ribosomal fractions upon ISR activation, while only 10% showed enrichment ( Fig. S1 A ). Among those, 2.3% were mitochondrial mRNAs and, accordingly, Ingenuity Pathway Analysis showed enrichment for mitochondria-related terms ( Fig. S1 B ). These findings were further validated in both BRAF mutant ( Fig. 1 D ) and neuroblastoma RAS (NRAS) mutant ( Fig. S1 C ) cell lines by performing polysome profiling followed by quantitative RT-PCR (RT-qPCR) upon salubrinal treatment. Since the influx of nuclear-encoded mitochondrial proteins from the cytosol directly regulates mitochondrial translation ( Richter-Dennerlein et al., 2016 ), the latter observation provides a likely explanation for the observed increase in mitochondrial protein synthesis.
Phenotype switching into an undifferentiated drug-tolerant state can be induced in vitro by activating the ISR, leading to an ATF4-dependent down-regulation of the microphthalmia-associated transcription factor (MITF; Falletta et al., 2017 ). Accordingly, exposure of drug-naive melanoma cells to salubrinal, an ISR agonist ( Boyce et al., 2005 ), increased levels of ATF4 and caused a concomitant down-regulation of MITF ( Fig. 1 A ).
We have now provided evidence that tetracyclines affect the growth of both mesenchymal and NCSC de-differentiated drug-tolerant cells in vitro. To assess the sensitivity of these and other drug-tolerant subpopulations in vivo, we treated Mel-006 with either D + Tige or DT until reaching MRD. Compared with DT treatment, the D + Tige combination successfully eradicated most of the NCSCs (NGFR + AQP1 + ), undifferentiated/mesenchymal-like cells (AXL + ), and SMCs (CD36 + ) drug-tolerant cells ( Fig. 4, A–C ). Similarly, in two different BRAF mutant PDX cohorts (Mel-006 and Mel-015) treated with the triple DTT combination, antibiotic treatment led to the eradication of NCSCs (NGFR + AQP1 + ), undifferentiated/mesenchymal-like cells (AXL + ) and pseudo-starved cell population SMCs (CD36 + ). The hyperpigmented cell population (MITF + MLANA + ) was the only drug-tolerant population to resist tigecycline combinatorial treatments ( Fig. 4, B–E ). Note that, consistent with tigecycline targeting mitochondrial translation and not metabolism, spatial metabolomics indicated that the antibiotic-containing treatment (DTT) did not induce any significant metabolic shift compared with DT alone ( Fig. S3, A–N ). These data indicate that a combination of antibiotics and MAPKis affects known drug-resistant populations by targeting mitochondrial translation in both de-differentiated (NCSCs) and undifferentiated/invasive states in the absence of significant metabolic rewiring.
To assess the relevance of our in vitro and preclinical findings, we followed the clinical course of one 73-yr-old female patient at our clinic. The patient was diagnosed with stage III melanoma in 2011 and with a relapse of her disease in 2016 after an episode of jaundice, which was related to a tumor mass in her gallbladder and bile duct. Histology and immunohistochemistry of the bile duct biopsy were performed ( Fig. 6 B ). H&E (left) shows a highly anaplastic tumor with large epithelioid cells and pleomorphic nuclei; the presence of brown pigment associated with these cells was highly suggestive for a melanoma metastasis. The immunostaining for S100 (right), one of the most sensitive markers to identify melanoma, was diffusely positive at nuclear and cytoplasmic levels, therefore confirming the diagnosis of melanoma metastasis. Baseline positron-emission tomography/computed tomography (PET-CT) showed metastatic tumor at the aforementioned locations as well as in the liver and in the gallbladder ( Fig. 6 C ). Subsequently BRAF-MEK inhibitor therapy was initiated. Response assessment after four cycles showed that while the liver metastasis had responded to the treatment, the gallbladder did not. Due to a skin infection (an acne-like rash) the patient received doxycycline during her fifth BRAF-MEK inhibitor cycle for a total of 12 d. Strikingly, the gallbladder metastasis started to regress after six cycles, as measured by CT scan, and the PET-CT scan after eight cycles showed a complete response. The patient was under BRAF-MEK inhibitor therapy and had a persistent response for >36 mo ( Fig. 6 C ). This particular case study highlights the potential clinical benefit of using tetracyclines to sensitize intrinsically resistant lesions to MAPK inhibitors.
Doxycycline is a broad-spectrum antibiotic that also belongs to the tetracycline family. It exerts its antibacterial action by binding to the 30S ribosomal subunit and thereby blocking ribosome biogenesis. It can be administered orally for extended periods of time with only minor adverse effects in patients ( Tan et al., 2011 ).
We also assessed whether tetracyclines can overcome intrinsic resistance to targeted therapy. To this end, we derived a cutaneous melanoma PDX model (Mel-007) from a lesion that exhibited intrinsic resistance to a combination of BRAF-MEK inhibitors. Exposure of a cohort of these mice to DT versus DTT showed that the addition of tigecycline promoted a more robust antitumor effect and even promoted tumor regression, in contrast to DT treatment ( Fig. 6 A ).
We postulated that the differential efficacy of the antibiotic combinatorial treatment in preventing the development of resistance between Mel-006 and Mel-015 BRAF V600E mutant melanoma PDXs may result from a difference in the kinetic and/or extent at which the ISR pathway is activated before applying the therapy. Consistently, ATF4 activation was readily detectable by western blotting, before the start of the therapy (T 0 ), in the Mel-006 PDX model, an observation that may explain the high sensitivity to the antibiotic treatment and the long-lasting response ( Figs. 1 G and 7 A ). In contrast, ATF4 activation could only be detected in lesions from Mel-015 following therapy exposure ( Figs. 1 G and 7 B ). Importantly, basal ATF4 levels were also detectable in drug-naive lesions from the tigecycline-sensitive models Mel-077 UM model and the Mel-020 and Mel-083 NRAS Q61R mutant models ( Fig. S5, A–C ). This observation may explain why the OS and PFS were comparable in cohorts exposed to the antibiotics at MRD or from the beginning of the treatment. These data suggest that the extent of the response to mitoribosome-targeting antibiotics is dependent on the level of chronic ISR activation. In keeping with this, cotreatment with the ISR inhibitor ISRIB, which blocks signaling downstream of the eIF2α kinase and thereby dampens ATF4 activation and ISR engagement ( Fig. S5 D ), reduced CHOP induction ( Fig. S5 D ) and abolished the apoptotic response observed in a series of melanoma cells lines exposed to doxycycline ( Fig. 7 C ). Consistently, silencing of ATF4 was also sufficient to overcome doxycycline-induced growth inhibition ( Fig. S5, E and F ). Altogether, these data indicate that dependency on mitochondrial translation is a consequence of ATF4-mediated ISR activation. Importantly, these findings also identify ATF4 as a predictive biomarker for the antitumor efficacy of the antibiotic treatment.
Cancer cells have the ability to survive a wide range of insults—including therapy exposure—through activation of an ATF4-ISR–dependent translation remodeling. We show herein that this pathway, in addition to promoting an overall decrease in cytosolic translation, enhances mitochondrial protein synthesis and selective translation of mRNAs encoding mitochondrial proteins in the cytosol and thereby establishes an unexpected vulnerability to inhibitors of mitoribosome assembly or function. Remarkably, this vulnerability can be targeted using the FDA-approved and widely used mitoribosome-targeting antibiotics. Accordingly, we show that tigecycline and doxycycline can decrease the growth and viability of a wide range of melanoma cells, exhibiting elevated ISR activity, including de-differentiated DTP cells or cells that have acquired resistance to targeted and immune therapies. We show that ATF4 inhibition or pharmacological inactivation of ISR rescues the antitumor effects of such antibiotics, thus confirming that this dependence relies on elevated ISR activity.
It has been proposed that internal ribosome entry site–dependent translation is one mechanism allowing translation of transcripts encoding survival proteins in cells exposed to stress and engaging an ISR. In fact, the translation of ATF4 itself depends on the internal ribosome entry site (Chan et al., 2013). Here we show that transcripts that are recruited to the ribosomes are enriched in rG4 sequences, raising the possibility that these elements also contribute to the selective translation of a series of transcripts, including those encoding mitochondrial proteins, in stressed cells.
Importantly, although providing a significant increase in survival, the triple DTT combination did not prevent relapse in another BRAF mutant preclinical PDX model (Mel-015). The relatively lower benefit from the tigecycline treatment in this model correlated with undetectable levels of ISR activation (as measured by lack of ATF4 expression) before treatment. ATF4 levels also predicted responses of therapy-resistant melanomas, such as UM and BRAF WT cutaneous melanomas, to the tetracycline treatment. These observations offer a new avenue for the treatment of these diseases with no, or only limited, therapeutic options and indicate that ATF4 levels are predictive of responses to tetracycline exposure, either as a single agent or in combination with standard of care.
Note that, in addition to their ability to inhibit mitochondrial translation, it remains possible that the antitumor effect of tetracyclines is multifactorial. Recent findings highlighted that mitochondrial translation deficiencies impair lysosome acidification and, thereby, autophagy (Yagi et al., 2021). Given the importance of autophagy in the biology of drug tolerance (Kinsey et al., 2019), this observation may also partly explain the efficacy of tetracyclines in delaying/preventing the development of resistance to MAPKi. Moreover, both dabrafenib and trametinib are partially metabolized by CYP3A4 (Lawrence et al., 2014), which is inhibited by tetracycline. Its coadministration may therefore raise the active concentrations of dabrafenib and trametinib and thereby enhance the antitumor efficacy of DT (Bassi et al., 2004). We also cannot rule out that, in addition to cancer cell intrinsic effects, the dramatic responses observed in the preclinical and clinical settings are a consequence of tetracycline-mediated remodeling of the tumor microenvironment, such as the (intratumor) microbiome. This may be important, as the efficacy of anti–PD-1 therapy has been shown to be affected by the microbiome (Matson et al., 2018; McQuade et al., 2019). However, most common symbiotic bacteria are resistant to doxycycline, which is a broad-spectrum antibiotic that can be administered orally for long periods of time with no or minor toxic effects (Tan et al., 2011). Its administration is therefore unlikely to affect significantly the patients’ microbiome.
In conclusion, our data indicate that the repurposing of mitoribosome-targeting antibiotics offers a new promising therapeutic avenue for the treatment of a large spectrum of melanoma patients, including those with limited therapeutic options. Moreover, we provide evidence that patient stratification should be guided by ATF4 levels, which could be used as an accompanying biomarker to predict efficacy. Importantly, this drug-repositioning strategy can be easily implemented in the clinic.